Keywords: sympathetic dominance, autonomic nervous system, chronic stress, parasympathetic balance, vagus nerve stimulation, PTSD, nervous system regulation, trauma recovery.
Introduction

In today’s high-stress environment, many individuals unknowingly operate in a prolonged state of sympathetic dominance—a chronic overactivation of the “fight or flight” response governed by the sympathetic nervous system (SNS). While short-term SNS activation is critical for survival, its long-term engagement without sufficient counterbalance from the parasympathetic nervous system (PNS) leads to widespread health consequences, both mental and physical. Understanding this imbalance is essential for addressing chronic stress, trauma, and burnout

What Is Sympathetic Dominance?
The autonomic nervous system (ANS) comprises two branches: the sympathetic and parasympathetic systems. The sympathetic branch prepares the body for perceived threats—raising heart rate, increasing blood pressure, halting digestion, and releasing cortisol and adrenaline. In contrast, the parasympathetic system promotes rest, digestion, and healing (Thayer et al., 2012).
Sympathetic dominance occurs when the body is stuck in an overactive sympathetic state for extended periods, often due to trauma, unresolved emotional stress, or ongoing environmental pressures. This dysregulation may go unnoticed for years until symptoms manifest as chronic health conditions.
Long-Term Health Effects of Sympathetic Dominance
Research shows that long-term sympathetic dominance contributes to a range of physical and psychological disorders, including:
- Cardiovascular disease: Prolonged SNS activation elevates blood pressure and heart rate, increasing the risk of heart attacks and strokes (Goldstein, 2013).
- Immune suppression: Chronic stress impairs immune function, leading to increased susceptibility to infections and delayed wound healing (Segerstrom & Miller, 2004).
- Digestive issues: Suppressed parasympathetic activity leads to irritable bowel syndrome (IBS), constipation, and poor nutrient absorption.
- Insomnia and fatigue: Constant vigilance disrupts sleep cycles and prevents restorative rest.
- Mental health disorders: Conditions like PTSD, anxiety, depression, and panic disorder often stem from or are exacerbated by nervous system dysregulation (van der Kolk, 2014).
How to Correct Sympathetic Dominance
Correcting sympathetic dominance requires an intentional shift toward parasympathetic activation, often called “rest and digest” or “feed and breed” mode. This shift can be achieved through a combination of lifestyle, therapeutic, and neurological interventions.
1. Breathwork and Vagus Nerve Stimulation
Deep, slow breathing—especially diaphragmatic breathing—stimulates the vagus nerve, which promotes parasympathetic activation. Techniques like box breathing, alternate nostril breathing, and 4-7-8 breathing are clinically proven to reduce cortisol and heart rate (Brown & Gerbarg, 2005).
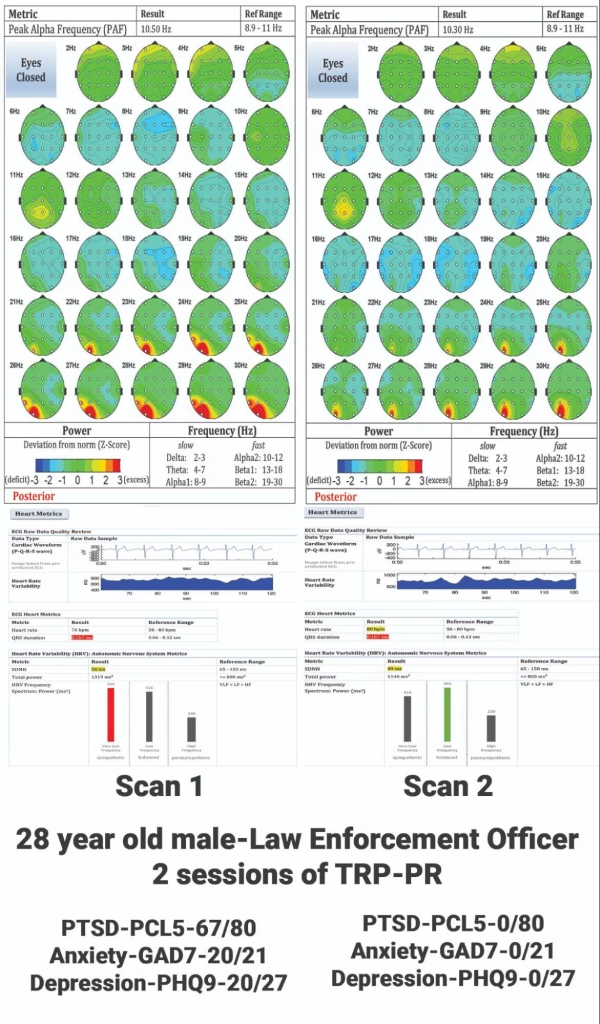
2. Neurofeedback and qEEG-Guided Interventions
Quantitative EEG (qEEG) brain scans can objectively measure sympathetic dominance through beta wave overactivation and underactive alpha/theta waves. Neurofeedback protocols retrain the brain into more balanced states, reducing hypervigilance and improving resilience (Hammond, 2011).
3. Trauma-Focused Protocols (e.g., TRP–Peer Rescue)
Innovative, non-clinical approaches like the Trauma Resiliency Protocol–Peer Rescue (TRP–PR) use neuro-linguistic programming (NLP), memory reconsolidation, and somatic regulation to downregulate sympathetic arousal and shift the body into a parasympathetic healing state. Studies underway at Arizona State University are measuring pre/post shifts using qEEG and Evox scans.
4. Mindfulness and Meditation
Mindfulness practices increase heart rate variability (HRV), a strong biomarker of parasympathetic health (Thayer et al., 2012). Consistent meditation also improves prefrontal cortex function, which helps regulate the limbic system and calm overactive stress responses.
5. Nutritional and Supplement Support
Chronic stress depletes essential nutrients like magnesium, B-complex vitamins, and omega-3 fatty acids—all vital for nervous system function. Anti-inflammatory diets and adaptogenic herbs (e.g., ashwagandha, rhodiola) support nervous system balance (Lopresti et al., 2014).
6. Movement and Nature Exposure
Rhythmic, low-intensity movements like walking, yoga, and tai chi promote vagal tone. Time in nature also reduces cortisol and SNS overactivity—often within minutes of exposure (Park et al., 2010).
Check out scoring changes with TRP-PR. https://healingthehero.org/resources/
Conclusion
Sympathetic dominance is not a character flaw—it’s a physiological survival response that, when uncorrected, becomes pathological. By integrating science-backed interventions that restore autonomic balance, individuals can experience significant improvements in physical health, emotional resilience, and cognitive clarity.
Healing the nervous system is not only possible—it’s essential.
References
Brown, R. P., & Gerbarg, P. L. (2005). Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression: Part I—neurophysiologic model. Journal of Alternative and Complementary Medicine, 11(1), 189-201. https://doi.org/10.1089/acm.2005.11.189
Goldstein, D. S. (2013). Adrenal responses to stress. Cellular and Molecular Neurobiology, 33(5), 625–632. https://doi.org/10.1007/s10571-013-0021-6
Hammond, D. C. (2011). What is neurofeedback? Journal of Neurotherapy, 15(1), 1–2. https://doi.org/10.1080/10874208.2011.545762
Lopresti, A. L., Hood, S. D., & Drummond, P. D. (2014). A review of natural remedies for treating early withdrawal symptoms of substance addiction. Drug and Alcohol Review, 33(2), 148–160. https://doi.org/10.1111/dar.12118
Park, B. J., Tsunetsugu, Y., Kasetani, T., Kagawa, T., & Miyazaki, Y. (2010). The physiological effects of Shinrin-yoku (taking in the forest atmosphere or forest bathing): evidence from field experiments in 24 forests across Japan. Environmental Health and Preventive Medicine, 15(1), 18–26. https://doi.org/10.1007/s12199-009-0086-9
Segerstrom, S. C., & Miller, G. E. (2004). Psychological stress and the human immune system: A meta-analytic study of 30 years of inquiry. Psychological Bulletin, 130(4), 601–630. https://doi.org/10.1037/0033-2909.130.4.601
Thayer, J. F., Åhs, F., Fredrikson, M., Sollers, J. J., & Wager, T. D. (2012). A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health. Neuroscience & Biobehavioral Reviews, 36(2), 747–756. https://doi.org/10.1016/j.neubiorev.2011.11.009
van der Kolk, B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. Viking.